Foot & Ankle
Select a treatment from the list below.
Warning: This information contains some graphic clinical photographs.
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
The Achilles tendon is a strong cord that attaches the calf muscles to the heel bone. It is used to push off with the foot when walking and running. Rupture of the Achilles tends to occur during sporting activity. The patient will often describe hearing a crack or feeling like they have taken a blow to the back of the heel. There is often marked discomfort and the patient struggles to walk.
Many patients have had previous problems with aching around the Achilles tendon due to degenerative changes within the tendon. These changes occur from the late thirties onwards. Ruptures classically occur in patients in their late thirties and forties as they remain physically fit and pursue high impact sports such as squash but have achilles tendonopathy.
Initial treatment involves icing the area and putting a half plaster cast on that keeps the toes pointed like a ballerina. The patient will need crutches and should not bear any weight on the affected foot. The next step is examination by an orthopaedic surgeon with a special interest in foot and ankle surgery and then an ultrasound examination will be performed to determine how close the two ends of tendon are. If they are less than 5mm apart then this means surgery is often not required unless the patient is an elite athlete.
If the ends are 5mm or more apart then surgery should be considered as the re-rupture rate is deemed to be higher if the foot is treated with plaster casts alone. Whether surgery is used or not does not change the length of time that the foot needs to be immobilized in plaster which will be seven weeks in total. Initially the foot will be fully pointed and the last plaster cast (there will be a minimum of three used to gradually bring the foot up to a neutral position) with the foot at right angles to the leg.
On removing the plaster cast, heel raises will be inserted into the patients shoes in order to offload the Achilles and physiotherapy will be started.
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Ankle arthroscopy is often referred to as keyhole surgery. The use of modern technology allows operations to be performed through keyhole incisions. `this has advantages over conventional surgery as the body responds badly to open incisions and complications of open surgery are higher.
Ankle arthroscopy is performed under a general anaesthetic and many procedures are performed as a daycase. During the surgery, a thin telescope (arthroscope) is inserted into the ankle joint, this allows the surgeon to see the inside of the joint and to operate on the soft tissues of the ankle and to remove bony spurs.
After your operation you will have a padded bandage in place. You will do no harm by gently moving your ankle within your bandages. Before you go home you will be seen by a physiotherapist that will give you advice regarding ankle exercises and how much weight you are allowed to bear on your leg.
Work
Return to work when you are confident that your ankle is comfortable enough to withstand the stresses of your job. If you are office based you should be able to return to work within seven days. If your job involves you being on your feet most of the day you may require two to three weeks off work.
Driving
Driving is usually possible about seven days after surgery as long as your ankle is comfortable and you are able to safely perform an emergency stop.
Complications
There is a small (about 1 in 600) risk of deep infection. A small number of patients will get some numbness or tingling on the top of the foot as a consequence of damage to very small nerves. Usually this is temporary but in some it can give rise to a permanent small numb or sensitised area.
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Osteoarthritis, or wear and tear, of the ankle is a common problem. It is more likely to have occurred if you have fractured your ankle in the past or if a family member has osteoarthritis of other joints. Most patients will complain of an aching pain along the front of the ankle joint which may be present at rest and at night if the wear within the joint is advanced.
In the early stages there are many conservative measures that can be helpful. Painkillers such as Paracetamol or Ibuprofen can be useful in taking the edge of the pain. In addition, Glucosamine and Chondroitin (available in health shops as well as on prescription) is sometimes beneficial.
The ankle is a weight bearing joint so weight loss will be helpful in reducing pain. Behaviour modification such as the reduction of high impact activities (running) and substituting this with cycling or swimming will reduce pain.
Wearing boots rather than shoes can offer more support to the ankle which may reduce pain.
Once the pain in the ankle becomes worse, and is not helped by the above measures, a corticosteroid injection into the ankle joint often helps to settle the pain down for anything up to a year. The response to injections is however variable and it may only help for weeks. It is also useful in confirming that the ankle is the sole source of your pain. This is particularly useful if any further surgery is considered. Key hole surgery can be employed to smooth off ragged cartilage (the smooth covering of the ends of your bones within the ankle joint which is damaged with osteoarthritis) and is also useful in reducing pain in the medium term.
In patients with severe pain then more major surgery can be beneficial. Ankle Fusion and Total Ankle Replacement (TAR) are both used for people with ankle arthritis. Ankle replacement has the benefit of giving the patient slightly more movement than a fusion (deliberate joining of the shin bone and talus foot bone that sits within the Ankle mortise) hence abolishing all movement and hence pain. Ankle replacement also protects the joints of the middle part of the foot which are more likely to become arthritic if a fusion is performed.
Fusion is a tried and tested technique whilst ankle replacement surgery continues to evolve, though modern implants have superior results when compared with their predecessors. Ankle replacements may fail, i.e. become loose and the components may migrate into abnormal positions. They would then need to be revised (often to a fusion) which would involve further surgery.
As a result, TAR is usually reserved for patients with inflammatory arthritis (such as rheumatoid arthritis) or more elderly patients with ankle arthritis.
Ankle Arthrodesis (Fusion)
This operation is performed for patients with Ankle arthritis that no longer responds to more conservative treatments or procedures. It can be done arthroscopically (keyhole surgery), if the ankle/foot position is not too deformed, or via an open operation if deformity needs to be dealt with as well. The bones are held in position by two or more large screws that fix the ankle in position and compress the two bone surfaces together to encourage fusion.
After surgery, you will be placed into a half cast (to allow swelling) and asked to keep your foot elevated at the level of your heart (putting it up on two cushions on a coffee table is usually adequate) for the first two weeks. You will then be reviewed in clinic at 2 weeks to check that all your wounds have healed and you will be placed into a new, complete, lightweight cast. You may be allowed to bear some weight at this stage but you will still be using crutches to ensure that only a small amount of your weight is transmitted through the operated on leg. A further review is arranged at 6 weeks and 12 weeks to ensure that the fusion is progressing, assessed clinically and by x-rays. At the 12 week point you should be able to bear all your weight through the affected leg whilst wearing a splint.
The minimum time for fusion is 3 months and it can take longer before your ankle is completely comfortable. The best result is often obtained about a year post-surgery.

Ankle joint arthritis

Ankle joint arthritis

A fused ankle joint

A fused ankle joint
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
The ankle joint attaches the foot to the leg. There are strong ligaments that attach from the shin bone (tibia) and fibula to the talus and calcaneum (heel bone). The lateral ligaments are frequently injured during sporting activity, when the ligaments are partially torn it is termed an ankle sprain. Ankle sprains are the most common musculoskeletal injury that presents to Accident and Emergency departments.
Ankle instability is most common in patients that have had previous ankle sprains. The ankle can give way when walking and may occur with the slightest unevenness of the ground. It can be painless, often if the ligaments are completely ruptured or painful if they are stretched. If the ankle is unstable there is a risk that arthritis can ensue.
Physiotherapy and ankle braces may be useful in controlling ankle stability and wearing boots rather than shoes is often more comfortable and provides additional support. Despite this conservative treatment surgical stabilization of the ankle may be required.
Ankle stabilisation procedures:
Modified Brostrom-Gould Procedure
This operation involves making a cut over the ligaments on the outer aspect of the ankle. The slack ligaments are cut and then repaired by “double-breasting” the ligaments which tightens them to the correct tension. The wound is closed using dissolvable sutures.
Following the operation, you will be placed into a half-cast with your foot held at right angles to the leg. You will be reviewed at two weeks to ensure that the wounds have healed and to convert the half cast to a completed cast. Partial weight-bearing can be commenced at this stage.
At six weeks following the operation the cast is removed and an ankle brace is worn in its place. Physiotherapy is commenced at this stage and at three months following surgery the ankle brace may be removed.
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Hallux Valgus (Bunion) corrective surgery
Patients with Hallux Valgus (Bunion) usually complain of a painful bump on the medial (inside) of the great toe (Hallux) metatarsophalangeal (MTP) joint. The hallux moves towards the second toe occasionally causing crossover of toes.
The tendons that pass under the metatarsal head have two bones within them (sesamoids). The best example of a sesamoid bone is the knee cap. Sesamoid bones are present when a tendon is likely to be but under great stress (60% of your bodyweight goes through the hallux MTP joint when walking). Over time, the metatarsal head falls medially off the sesamoid platform, leaving the lateral sesamoid uncovered. The tendons attached to the hallux pull the toe into further valgus and worsen the metatarso-sesamoid subluxation.
Ultimately, the weight bearing function of the great toe becomes compromised and lateral metatarsalgia (forefoot pain) may result as weight bearing is transferred laterally.
The operation aims to reposition the metatarsal head over the sesamoids and restores the normal weight bearing properties of the metatarsal. By narrowing the intermetatarsal angle (and removing the medial bump), it reduces the forefoot splaying as well as the overall width of the forefoot.
The following diagrams demonstrate how the metatarsal head is moved medially and fixed using special screws.
Post-operative rehabilitation
Weight bearing is allowed in a flat post operative shoe for the first 6 weeks. However, patients are advised to keep the foot elevated as much as possible for the first 2 weeks. Sutures are removed after 10-14 days and the patient taught to do perform their own bandaging and encouraged to mobilise the great toe.
Radiographs are performed after 6 weeks to check the position of the osteotomy and the progression of union. At this point the flat post operative shoes are discarded and the patient commences in normal footwear.
The foot is likely to be sore for the first three months following surgery and that the result depends upon compliance with the post-operative bandaging and mobilisation regime. In addition, you may not be able to wear a shoe comfortably until 16 weeks and that the full recovery (including the resumption of sport) may take up to 12 months.
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Osteoarthritis of the great toe (Hallux) metatarsal-phalangeal joint (MTPJ) presents with stiffness of the great toe, some swelling, and pain. Impact activities such as running usually exacerbate the symptoms. It can be caused by previous trauma to the big toe, inflammation within the joint, or may develop without any obvious precipitating cause.
Treatment options include simple analgesia and activity modification, shoe modifications, injections, cheilectomy (removing some of the bony lumps and worn areas of the joint), fusion (making the joint stiff), and joint replacement.
Cheilectomy aims to improve the range of MTP joint dorsiflexion by excising dorsal osteophytes from the head of the metatarsal and base of the proximal phalanx. In removing these abnormal bone growths from the margins of the joint, and the most worn portions of the joint surfaces, the joint is often more comfortable, but not always pain free. The recovery from this operation is quicker than a fusion.
Sutures are removed after 10-14 days and early range of motion exercises are encouraged. Patients may weight bear as tolerated and aim to wear a normal shoe after 6 weeks. As a general rule you will retain approximately half the extra range of dorsiflexion that is achieved at the time of surgery. If the surgery is not as successful as hoped, then a fusion operation can be performed at a later date.
Fusion surgery aims to make the big toe joint permanently stiff, and therefore abolishing all pain from that joint. It is currently the gold standard operation for an arthritic big toe joint. The joint becomes solid so the joints proximal and distal to the fused joint will adapt to allow more movement within them. The toe is fixed in a slightly elevated position to allow normal walking and the use of a small court shoe if required. High heels will not be possible. Patients quickly adapt to the fusion and walk normally, with some patients achieving a high level of function such as recreational running and a return to sporting activities.
The arthritic joint is excised and the two bones are then fixed temporarily with a smooth wire and then fixed using two crossed screws or a plate and screws. The wound is closed using dissolvable sutures. Post operatively the foot should be elevated for 24-48 Hrs. Walking is permitted, but only in the rigid flat post operative shoe, for 6 weeks. Suture ends are trimmed off at 2 weeks.
The foot is X-rayed at 6 weeks and if satisfactory normal shoes can now be worn. A final x-ray at 12 weeks is required before full impact activities (running, dancing etc.) can resume.

Plate and screw fusion 1st MTPJ for hallux rigidus
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Heel pain can be caused by a variety of conditions but the commonest cause is plantar fasciitis. Other causes include insertional achilles tendinopathy, Haglund deformities and bursitis, tarsal tunnel syndrome, and insufficiency fractures of the heel bone.
Plantar Fasciitis or Policeman’s heel is a painful condition typified by pain felt on the sole of the heel, often worst on the first heel strike in the morning (start-up pain). It may also become worse as the day wears on particularly if the patient has a job that involves a lot of walking. It is often due to inflammation of the plantar fascia as it attaches to the calcaneum (heel bone). The precipitating cause is often not known, but it can be associated with other inflammatory conditions, and in some cases can be linked to an overly- tight calf muscle/ achilles tendon complex.
The plantar fascia is a thick band of fibrous tissue on the sole of the foot which lies deep to the thick skin of the sole of the foot. It connects the heel bone to the base of the toes and provides support to the longitudinal arch of the foot.
This condition usually gets better with time but this can take many years. In the meantime, there are other treatments that can be employed to reduce the level of symptoms. Orthotics are insoles that can be worn within normal footwear. Heel raises with gel centres can be useful in offloading the painful heel.
Physiotherapy aimed at improving the strength of the small muscles within the foot has also been shown to reduce pain in plantar fasciitis. Eccentric stretching exercises stretch the calf and plantar fascia and are particularly beneficial.
If these conservative measures do not help, then an injection around the insertion of the plantar fascia can be performed. This can be done in conjunction with an ultrasound of the area to confirm the diagnosis. These injections can be repeated and sometimes multiple injections are required in order to settle the pain.
If patients fail to improve with these treatments, then shockwave therapy (ESWT) is a useful adjunct. It is carried out as a clinic based procedure over 3 appointments. See NICE guidance for further information:
http://www.nice.org.uk/guidance/ipg311/informationforpublic
If the calf muscle/ achilles tendon is overly tight then a lengthening procedure can be carried out as a day surgical procedure.
In rare circumstances, a surgical release of the plantar fascia can be performed in order to reduce pain. As this procedure is not guaranteed to reduce pain, and carries a small risk of damaging the small nerves that supply the sole of the foot with sensation, it is only employed as a last resort.
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Ingrowing toenails most frequently affect the big toenail and are caused when the sides of the nail grow into the surrounding skin. The skin subsequently becomes red, inflamed and tender. Bleeding and secondary infection can occur, with pus coming from the area.
There are a number of causes including:
- Curved or fan-shaped nails that predispose to cutting into the skin.
- Cutting the nails too short or curving them at the leading edge corners.
- Excessive pressure on the skin at the corners due to tight ill-fitting shoes.
The aim of toenail operations is to remove the side portion of the nail that is “ingrowing”, or to completely remove the nail, so that that portion or the whole nail does not re-grow.
Under local or general anaesthetic, the side portion of nail, or whole nail, is gently lifted off the nail bed and small oblique incisions are made in the proximal nail folds. The germinal matrix (where the nail grows from) has a chemical (phenol) applied to it that prevents the nail re-growing in that area. Sutures are inserted to close the wounds and the toe is dressed in a bulky dressing.
Post operative rehabilitation
The foot should be elevated for 24-48 hours. Weight bearing is permitted, as comfort allows. The dressings should be changed at 48 hours and replaced with a smaller, lighter dressing. The sutures should be removed at 10-14 days.
If the wounds continue to ooze, then they should be bathed daily in warm salty water. Antibiotics are only required if the toe becomes red and inflamed, or if pus is present.
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Curling of the lesser toes is quite common and may lead to a hammer toe or claw toe deformity. There are numerous causes as to why the toes may slowly and progressively develop such deformities, but essentially there is an imbalance between the pull of the extensor tendons, (on the top of the toe) and the flexor tendons (underneath the toe). Once the toe becomes deformed it can become uncomfortable in shoes as the knuckle can become prominent and then rub. Sometimes the tip of the toe may curl downwards instead of pointing forwards, which is also uncomfortable.
Most of the time they can be managed conservatively by modifying footwear or applying padding to the toe, but occasionally they require surgery to correct the deformity and relieve pain. The procedure usually involves a combination of tendon lengthening, or transfer, and a bony procedure to either fuse some of the small joints within the toe, or excise a joint.
A wire may be passed down the toe to hold the bones straight while the joints “knit”. This will be left in situ for 6 weeks, with a small portion extending from the end of the toe. The toe will need to be kept clean and dry for this time, before the wire is pulled out in clinic. Steri-strips (butterfly stitches) may be applied to the toe to assist in keeping it straight.
Post-operative rehabilitation
Steri-strips and sutures and are removed after 14 days. If taping was required, patients will be taught how to do this and will need to continue this daily for 6 weeks. Patients may weight bear as tolerated in post-operative shoes, but should elevate the foot for the first 24 Hours. Ankle exercises are encouraged, but you should not attempt to wiggle your toes. The aim is to wear a normal shoe after 6 weeks.
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Flat feet are common with 30% of the population having a flexible flatfoot (ie one that will correct into a normal shape, with a medial longitudinal arch, on tip-toe standing). Children may have this problem but frequently have no problems with normal activities and consequently can be left alone. Occasionally such a foot may ache with impact activities, and an insole may help with this symptom. The insole will not however permanently alter the shape of the foot. Most adults who grow up with flat feet manage perfectly well with normal shoes during all activities.
A fixed flat foot deformity (which does not correct on standing on tip-toes) is nearly always pathological and is more likely to require surgical intervention. A foot that was normal shape, but has become flat, is also pathological.
The feet are clinically examined and x-rayed to assess whether there is a requirement for orthotics, physiotherapy, or surgery, but the majority of flatfeet will require no treatment. If surgical treatment is required further scans (CT or MRI) may be undertaken to gain more information and allow surgical planning.
The type of surgery varies depending on the cause of the deformity, but can involve excising a coalition (an abnormal connection between bones), osteotomies (cutting and moving bones), tendon transfers, and fusing joints.

A flat left foot with a collapsed medial arch and valgus heel
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Morton’s neuroma is a swelling of the digital nerve (nerve that supplies sensation to the toes) just before the nerve splits into two to supply the webspace (opposing halves of two adjacent toes). Frequent complaints are of pain on bearing weight under the forefoot, which may be relieved on removing footwear. There may be abnormal sensation (pins and needles or numbness) in the webspace or in the toes, and the sensation of treading on a small marble.
Neuroma are usually suspected after taking a history and a clinical examination. An ultrasound or an MRI scan is usually used to confirm the diagnosis.
Treatment options include avoiding impact activities, altering shoe types, orthotics (insoles) and steroid injections around the nerve. If these fail then the swollen portion of the nerve can be excised.
A Morton’s neuroma can be approached via a dorsal or plantar approach. The dorsal approach divides the deep transverse ligament but may have fewer problems with wound healing and scar-related discomfort. A dorsal longitudinal incision is begun over the centre of the web space (between the MTP joints) and extended approximately 5cm proximally. The neuroma is then removed along with a small section of nerve both proximal and distal to it. This ensures complete removal of the neuroma. The specimen is then sent to the histology laboratory (to confirm diagnosis) and the wound closed with a dissolvable nylon sutures.
Post-operative rehabilitation
Although weight bearing is allowed in the flat post surgical shoe, it is recommended that you keep the foot elevated as frequently as possible during the first few days. Walking long distances should be avoided until wound healing occurs. This is important as it reduces swelling and prevents bleeding into the interspace. The suture ends are removed at 2 weeks and the patient is encouraged to mobilise as comfort allows after this in normal, spacious, flat shoes. Impact activities, such as running, dancing etc should be avoided until at least 6 weeks.
Numbness over adjacent sides of the toes is an inevitable consequence of removing the common digital nerve.
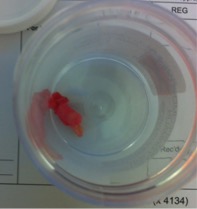
Morton’s neuroma excision, and the excised swollen nerve
Performed by – David Hinsley, Ngwe Phyo, Nick Ward
Chronic pain is often caused by inflammation and calcification of tendons (tendonitis) and their attachments to bone (enthesiopathy). This can occur due to sports injuries, overuse and the natural effects of aging.
Examples of common conditions we can successfully treat include Tennis and Golfer’s elbow (epicondylitis), shoulder pain (due to calcific tendonitis), hip pain (due to trochanteric bursitis), knee pain (due to patellar tendonitis), Achilles tendon pain (tendonitis), heel pain (plantar fasciitis/Policemans heel).
Extracorporeal Shock Wave Therapy (ESWT) is performed by Orthopaedic Surgeons in outpatients. This avoids the need for painful injections, medication or surgery. It is effective for many musculoskeletal problems even if other therapies have proved ineffective.
Shock wave therapy is the application of high energy focused sound waves onto the injured area. The technology was first developed for breaking up kidney stones without surgery known as lithotripsy. It soon became apparent that this level of focused energy promotes new blood vessel formation and natural healing in inflamed tissue. In other words, the shock wave can stimulate the healing of tissue which has not healed spontaneously.
A course of treatment usually requires at least three sessions, each taking about 10-20 minutes. Partial pain relief is often felt immediately following treatment and permanent results can be expected 4 – 6 weeks following the last session.
The chronic problems that can be treated using this therapy are common in many types of sports including golf, tennis, cricket, squash, running, rugby, football, hockey and athletics. They are also common in water sports enthusiasts especially, windsurfers, kite surfers and water skiers. They can also be an occupational hazard in manual workers. Interestingly they also can also occur from minor repetitive trauma such as house work and using a computer mouse!
Success rates of approximately 80% have been found in most studies investigating its effect.