
Shoulder & Elbow
Select a treatment from the list below.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
Shoulder arthroscopy is commonly known as keyhole surgery. It involves a camera attached to a thin telescope that is inserted into the shoulder via a small incision. With the camera, the surgeon can look inside the shoulder itself and identify any problems. If the camera reveals any problems the surgeon can use small instruments that can be inserted via another incision into the shoulder.
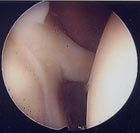
View inside a normal shoulder
Common shoulder problems that are treated by arthroscopic surgery include subacromial impingement, labral tears and worn articular cartilage.
In addition, complex surgery such as Rotator Cuff Repair and Shoulder Stabilisation can be performed using keyhole surgery techniques.
What happens in surgery?
The surgery in generally performed as a day case under a general anaesthetic. The operation usually takes around 30 minutes to perform although the time taken may be longer for more complex procedures.
At the end of the operation your shoulder is injected with a local anaesthetic to minimise the post-operative pain. The small wounds are closed with a stitch or steristrips. Your arm is rested in a sling for a few days (longer if more complex procedures are performed) and you can return to driving and other activities as comfort allows.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
This operation is performed for subacromial impingement, a condition that causes pain in the shoulder. In most instances, the pain is related to movement of the shoulder, particularly when the hand is raised above shoulder height.
Subacromial impingement is frequently related to sport, especially swimming and racquet sports, but also domestic tasks such as ironing and gardening. Pain caused by subacromial impingement commonly affects routine daily tasks such sleeping and dressing.
The pain is related to four tendons that move the shoulder. These tendons are collectively called the rotator cuff. They are attached to the shoulder blade at one end and to the top of the humerus (upper arm) at the other. The tendons pass through a narrow space just before attaching to the top of the humerus and it is this gap that can become narrowed over time due to a bony spike developing or a thickened ligament. This creates increased pressure on the rotator cuff tendons causing the pain of subacromial impingement.
Non-Operative Management
The initial treatment is usually rest, avoiding any activities that exacerbate the pain and the use of simple painkillers and physiotherapy. If the pain persists a steroid injection may then be recommended.
Prior to proceeding to surgery it is usual to perform X-rays or an MRI scan to ascertain the degree of damage.
Operative Management
The operation is carried out under a general anaesthetic and usually involves one night in hospital. The procedure is performed using two small incisions through which an arthroscope (telescope) and small instruments can be passed. These instruments are used to remove bony spikes, release tightened ligaments and increase the space through which the rotator cuff tendons pass.
The small wounds are closed with stitches or steristrips and your arm will be placed in a sling.
What happens after surgery?
Following surgery, exercises are started immediately to regain function in the arm. Physiotherapy is started after 2-3 weeks.
It will take between 3 weeks to 3 months for the shoulder pain to settle and function can continue to improve for 6 months after surgery.
You will need 2 weeks off work after surgery and longer if you have a manual or physical job. You should be able to drive after 2 weeks and gradually return to sport as comfort permits. About 80% of people who undergo a subacromial decompression find their pain and movement greatly improved by the surgery.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
There are 4 tendons that move the shoulder. These tendons are collectively called the rotator cuff. They are attached to the shoulder blade at one end and to the top of the humerus (upper arm) at the other end. They pass through a narrow space just before attaching to the top of the humerus. This space can become narrowed further over time due to either a bony spike developing or thickening of a ligament.
This causes increased pressure on the rotator cuff tendons, initially they get inflamed and painful, but if the pressure is not relieved the tendons can get damaged and ultimately they can tear. Normally the uppermost tendon, supraspinatus, tears first and if the tear gets worse the next tendon, infraspinatus, tears as well. The treatment depends upon the size of the tear.
Operative Management
Generally, an MRI scan is done before performing surgery. At the time of surgery, a subacromial decompression is performed first to help relieve the pain associated with the tear.
Small tears can be treated by arthroscopic repair, repair through a small incision or if very small can be left alone. This can be done with an overnight stay in hospital.
Larger tears generally need to be repaired and both arthroscopic and open techniques are used depending on the precise size and location of your tear. Arthroscopic repairs will involve the use of suture anchors (dissolvable plastic pegs with strong sutures attached) which are placed into the bone and the tendon is then sutured down to the anatomic insertion site. Typically, there will be between 3 and 5 small incisions to allow this surgery to be performed.
For open surgery 4-8cm incision is made on the side of the shoulder and the torn tendon reattached to bone with sutures. This requires a stay in hospital of 1-2 nights.
Pain in generally controlled by a nerve block in the base of the neck. Post operatively your arm will be placed in a sling, which will be needed for up to 6 weeks.
Post Operative Management
The first 3 weeks are spent with your arm in a sling with minimal movement. The aim of this phase is to allow the repair to heal strongly. Between 3 and 6 weeks physiotherapy is started to regain movement in the shoulder, which will be quite stiff by this time. You should be able to restart driving after about 2 months. The final phase is between 8-16 weeks. Strengthening exercises are started as the repair is now strong enough.
After 4 months some sports can be restarted, but heavy lifting and contact sports should be avoided until 6 months after surgery.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
The shoulder is the most commonly dislocated joint in the body. Some people develop recurrent problems with either repeated dislocations or the feeling that the shoulder is about to dislocate. This commonly occurs in people in their late teens or early twenties and may also cause pain in the shoulder.
The initial dislocation is usually related to an accident, commonly in sport, and causes damage to the rim of the joint, which does heal properly and leads to a long-term weakness. Physiotherapy may make the shoulder more stable but may not prevent further dislocation. If the symptoms interfere with everyday activities or sport reconstructive surgery can be indicated.
Prior to reconstructive surgery an MRI scan may be carried out, but commonly surgeons will recommend arthroscopy to determine how unstable the joint is and whether there is any damage to the joint. Stabilisation can be performed under the same anaesthetic as the arthroscopy.
Operative Management
Stabilisation can be performed arthroscopically and involves fixing the rim of the joint with absorbable tacks. But for more unstable shoulders open surgery may be required.
Open surgery is performed through a 5-10 cm incision on the front of the shoulder and the rim can be reattached as well as tightening the loose tissue at the front of the joint, which has been stretched by the recurrent dislocations.
Arthroscopic stabilisation can be performed as a day case or overnight stay, whereas open surgery will require a 1-2 night stay in hospital.
After surgery your arm will be placed on a special sling, which holds your arm close to your body. You will need this for 4 weeks.
Post Operative Management
You will need to wear a sling for up to 6 weeks, during this time you will not be able to lift, drive or perform any activities that may damage the repair. However, you will be able to start to move your arm under the supervision of a physiotherapist.
After 6 weeks you will be able to discard the sling and start to regain movement in your shoulder, avoiding strengthening exercises as the repair is not strong enough at this stage.
After 12 weeks the repair is strong enough to allow strengthening exercises. These are continued until 6 months after surgery. Most sports can be restarted after 6 months but for revision procedures or certain high risk sports this may need to be delayed further.
Success and Complications
About 90-95% of people with damage to the rim of the joint will have complete resolution of their symptoms and will be able to return to sports at their previous level. Failure is related to amount of damage to the joint detected at the time of surgery. As with all surgery there is a risk of infection, but this is about 1% and can generally be treated with antibiotics.
In some patients the main problem is laxity of the joint rather than damage to the rim. Although an operation may be indicated the success rate is lower.
In a few patients the problem is related to abnormal muscle activity. This is not suitable for surgery but is treated by specialised physiotherapy.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
Shoulder replacement has been an established treatment for many years now with a proven track record in terms of safety, satisfaction and durability. The procedure involves the replacement of the ball joint of the humerus at the shoulder with or without the replacement of the shoulder socket.
When is it done?
Shoulder replacement is performed for arthritis of the shoulder or after fractures of the shoulder which cannot be repaired. The main reason for surgery in arthritis is to relieve pain but stiffness or loss of movement may also be improved.
What does surgery involve?
The operation is usually performed under general anaesthetic but you may be offered a nerve block injection as well. The surgery is performed through a short incision 8-10 cm long at the front of the shoulder. One of the muscles (subscapularis) and the capsule are lifted off the joint and the ball joint is then exposed. Depending on the degree of arthritis present the ball joint can be either resurfaced with a metal cap or cut off and replaced with a metal stem and new ball joint.
The muscle and capsule are repaired back to the bone or secured by sutures through the new joint replacement and the skin is then closed, typically with a dissolving suture.
Post Operative Recovery
Typically, you will only need to stay in hospital for 1 or 2 days after your operation. After surgery you will be placed in a sling for about 4 weeks and then start physiotherapy exercises. it will take between 2 and 3 months to get the movement back and during this time you may not ba able to drive or work.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
Frozen shoulder or adhesive capsulitis is a very painful condition of the shoulder. It is common in the 35-55 year old age group and is not usually related to injury. The striking features of the condition are the combination of severe pain, especially at night or rest, along with marked stiffness of the shoulder with loss of rotational movement such as placing a hand behind your back. The condition foes through three stages, known as the freezing, frozen and thawing phases. Each phase typically lasts between 6 and 9 months but sometimes this timeframe is extended.
Cause
The cause of this condition has not been fully explained but there are changes which have been identified in the joint capsule which cause it to thicken and contract. The capsule is the lining of the joint which is normally quite loose and elastic to allow movement in all directions. When it becomes inflamed it will thicken up and became irritable causing pain. The thickened joint capsule retracts into itself and effectively shrinks the size of the joint lining which in turn limits the movement.
During the freezing stage, there is an increasing degree of pain, often described as a burning sensation over the outside of the shoulder joint. This is accompanied by a steady reduction in the range of movement until the arm can only really be moved by rotating the shoulder blade against the rest of the body.
The frozen stage follows and is most notable for the severe limitation of movement. However during this period, the pain has usually reduced or gone completely so that itis often not a major feature.
The thawing phase will then take place with a slow return of movement over several months. The first movement to return is lifting the arm forward (elevation) then sideways movement (abduction) and lastly rotation.
The condition is commoner in people who have diabetes and they can suffer from the condition in both shoulders at the same time in the most severe cases. Diabetics also tend to take longer to recover.
Treatment
The main effort in treatment is initially to reduce or stop the pain and then to restore movement. In the early stages the changes can be reduced or even reversed by an injection of steroid and local anaesthetic into the joint. Due to the thickening of the joint capsule and the inflamed nature of the joint it is usually uncomfortable to have an injection but it can speed the recovery in acute cases.
Surgery may be offered either to treat pain or restriction of movement and is usually a keyhole procedure where the joint is inspected using a telescope and the inflamed lining is released from the inside out using a cutting probe placed through a second keyhole at the front of the joint. The most critical area of thickening has been shown to be the rotator interval, a gap between 2 of the muscles of the rotator cuff, and releasing this has good results with movement and function being restored in most cases.
After surgery for a 2-4 weeks there may be more pain present as we encourage aggressive early mobilisation to restore function. If the shoulder is rested too much after surgery for frozen shoulder, then there may be a return of stiffness.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
This is a painful inflammatory condition which is noted for pain and loss of power at the elbow. The pain is felt over the origin of the muscles which extend the wrist and forearm. Usually it is not associated with any alteration in sensation but has pain which gets worse with resistance when bending the wrist back against pressure or resistance. Despite its name it is not directly associated with tennis players but can occur after an injury or a change in activity.
Treatment
The initial treatment should be the cessation of the painful activity if possible and rest for up to 6 weeks. If it does not settle by rest, then physiotherapy or a structured exercise programme may help.
Splintage
There are a number of different patterns of splints available on the market which have a varied effectiveness. In general, the clamp type of splint can be more effective as it offloads the injured tendons to allow them to recover. The splint will however need regular adjustment during the day to maintain effectiveness and may not be suitable in manual workers due to constant movement of the arm.
Steroid Injection
An injection of steroids (eg Cortisone) into the affected area can reduce symptoms or even eliminate them altogether. However often the pain returns after a few months if activity modification has not taken place.
Surgery
In those conditions which do not settle with all other treatments we would consider surgery. The operation can be done under a general or local anaesthetic (depending on suitability) and is a day case procedure. It involves identifying the damaged portion of the tendon and excising it along with a release of the tendon around the damage to reduce the tension on the remaining tendon structure.
Results of Treatment
The outcome after treatment for tennis elbow is not always successful. In general terms about 70% of people recover at each stage. That is, 70% get better by resting alone. Of the 30% who do not improve, 70% get better by physio. Of those who do not recover, 70% improve with injections. This also applies to surgery with approximately 70% getting a full or near full recovery from surgery. Of the remainder, 20% will improve but still have some symptoms and the remainder do not improve.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
This condition follows a similar pattern to tennis elbow but has the added complication of the close association of the ulnar nerve to the affected area. There are two main patterns of golfer’s elbow, those with no nerve involvement and those who have symptoms of numbness or weakness in the forearm and hand, particularly affecting the ring and little fingers.
Treatment is similar to tennis elbow with a graduated approach using rest, splintage, physiotherapy and surgery with the slight difference that where the ulnar nerve is also involved, the nerve should be explored and decompressed as required.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
OK Procedure
The Outerbridge and Kashiwagi procedure (usually shortened to OK) is a technique used to improve pain and movement in a stiff elbow or to remove loose bits of bone from inside the joint.
When is it performed?
A patient may complain of reduced movement or locking of the elbow. This may be painful and may be related to a background of an injury in the past. Loose bits of bone may be moving inside the joint and they will intermittently become stuck limiting movement. The joint may also have some elements of arthritis and spurs of bone can catch at the back of the joint over the tip of the elbow known as the olecranon.
How is it performed?
It is usually performed under a general anaesthetic using a tourniquet on the arm. The operation takes around 45 minutes to perform. A short incision is made at the back of the elbow and the triceps muscle is split lengthways to gain access to the olecranon. Any loose bone can be removed directly from the back of the joint at this stage. The olecranon tip is then exposed and any spurs of bone caused by arthritis are removed. This should restore the ability of the elbow to straighten. A small hole is then made directly through a thin plate of bone in the lower end of the humerus. Through this hole, access is available to the front of the joint and loose bone can usually be removed through this hole.
The bone that is removed to make this window through the joint is not load bearing and there is no major risk of fracturing the humerus by making a hole at this point. The joint is then washed out to remove any small debris and the triceps muscle is repaired before the skin is closed using absorbable sutures. After surgery you will use a sling for 1 or 2 weeks only for comfort and you will be encouraged to mobilise early with a physiotherapist.
Outcome
This operation is generally successful with high levels of patient satisfaction and improvements in movement. However, in more arthritic joints the movement may improve but the pain may still be present and further more major surgery may be required such as joint replacement.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
Total Elbow Replacement
This procedure is performed for stiff arthritic elbows where the range of movement has become limiting or the pain in the elbow has become too severe for daily activities. The operation consists of the cutting out the natural joint and the replacement of that with an artificial metal joint. The artificial joint has 2 components, the humeral component and ulna component which are inserted to the relevant bones. The may be secured using bone cement or some replacements can bond directly to your natural bone. The 2 components then link together with a plastic bearing surface to allow free movement at the new joint.
The operation takes about 1 1/2 hours to perform and you would typically stay in hospital for 2 days after surgery. You will be encouraged to mobilise early but you may have a plaster cast or brace fitted for the first 2 weeks to protect the muscles and soft tissues after the operation. Following this you will undertake a rehabilitation programme aimed at maximising strength and function.
Typically, it may be 6 weeks until you have sufficient function to return to driving.
Total Elbow Replacements have a planning life of around 10 years after which the may need a second replacement fitting if symptoms recur or the plastic bearing wears out.
Performed by – Gareth Hill, Phil Rosell Ankit Desai
This is a smaller operation which is performed to replace either an arthritic joint or after an injury if the radial head is too badly damaged to be repaired. The operation takes around 45 minutes and consists of a short incision on the outside of the elbow and opening up the lateral side of the joint. The radial head is the part of the joint which is involved in forearm rotation and this can be replaced quite easily by cutting the neck off the bone and then inserting a new metal or ceramic head onto a short stem placed down the middle of the bone. Again this can be fitted using cement or press fit/ direct bonding techniques.
After surgery you will be encouraged to mobilise early and restore the movement of the elbow.
Post operative stiffness is a recognised complication of elbow replacement and it is not unusual to have an end result with a range of movement of 30 to 130 degrees. That is the elbow will not go fully straight and you may lose 30 degrees of that straightening. However, the range achieved after replacement surgery is usually sufficient for all activities of daily life

